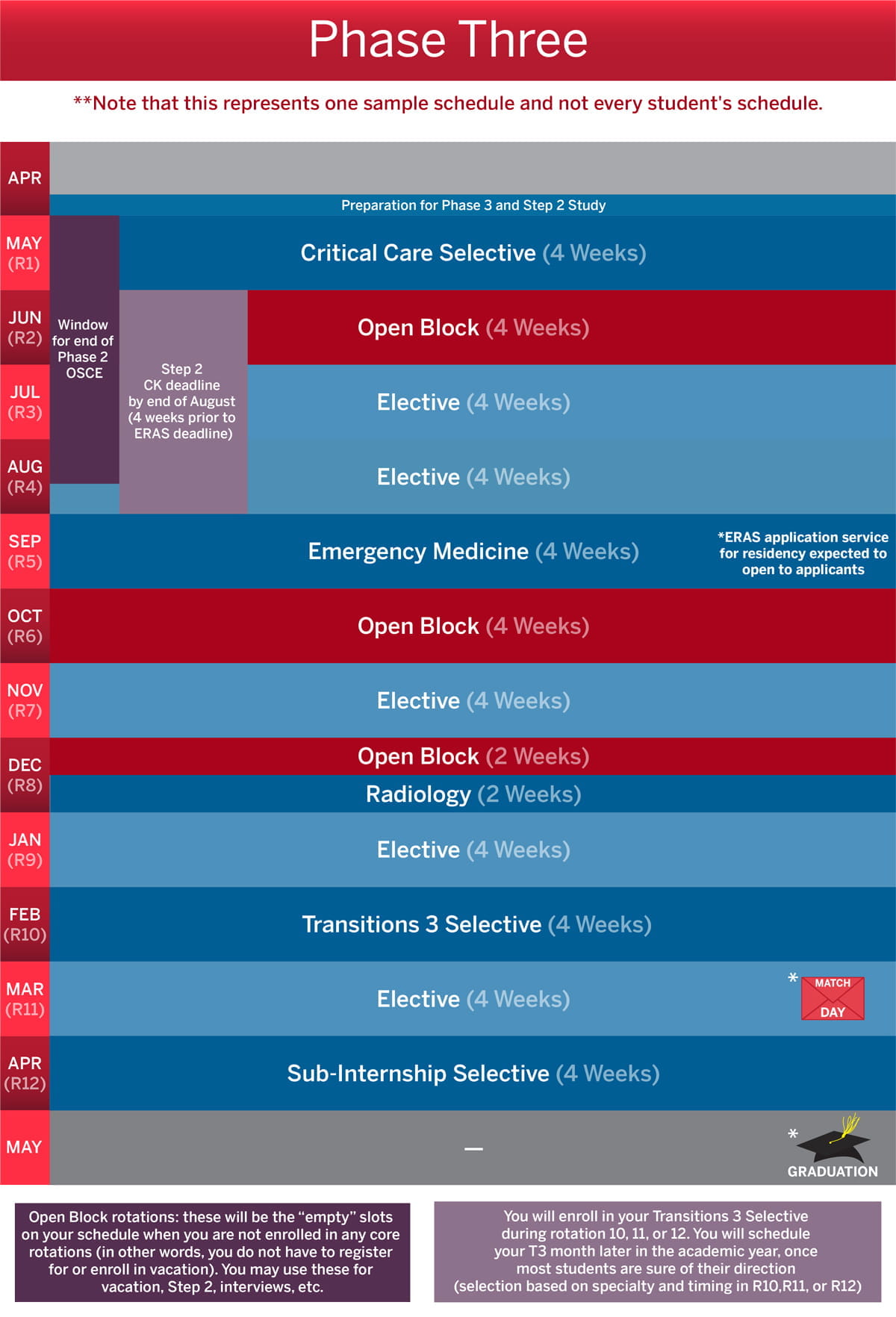
Phase 3 of the MD curriculum builds upon the foundational skills developed during Phase 1 and Phase 2 to prepare IU School of Medicine graduates for supervised clinical practice, scholarship and service in residency and beyond. This phase includes required core clinical rotations, tailored electives and the residency-preparation course, Transitions 3. For participants in the optional Scholarly Concentrations program, students also have time to complete their scholarly project and scholarly product and participate in IU School of Medicine Education Day, if not done previously.
Jump to:
Important Reminders Graduation Requirements Enrollment Requirements Open Block Phase 3 Rotations
Sub-Internship Selective Critical Care Selectives Electives Transitions 3 Scholarly Concentration Program