The first two years of medical school focus on developing foundational science knowledge and integrating that knowledge with clinical skills. Phase 1 courses are designed to advance competency in medical knowledge with an emphasis on the basic sciences to form a foundation for clinical competency.
Important COVID-19 Information
Find ongoing updates due to COVID-19.
UDOS = Understanding Diseases of Organ Systems
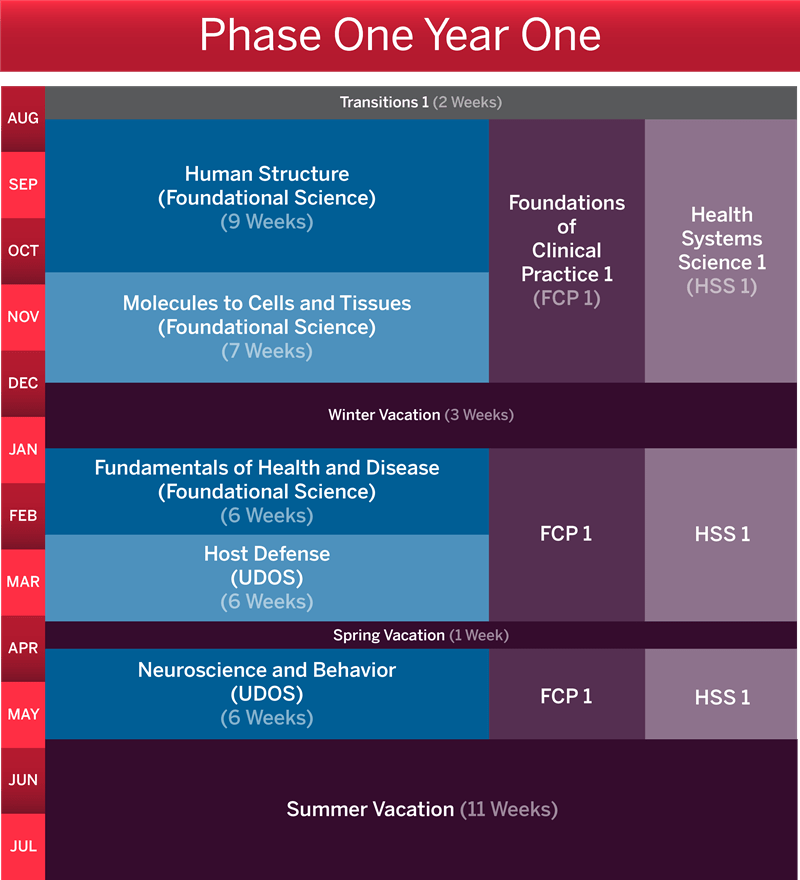
Transitions 1 takes place for two weeks at the beginning of August.
Foundations of Clinical Practice 1 and Health Systems Science 1 run for the whole year, except during vacation breaks.
In mid-August, students begin Human Structure, which runs for nine weeks. In late October, the seven-week Molecules to Cells and Tissues course begins.
In mid-December, students have a three week winter vacation.
In mid-January, courses resume with Fundamentals of Health and Disease for six weeks. In late February, students take the Host Defense course for six weeks.
In early April, there is one week of spring vacation.
The final course of Phase One Year One is Neuroscience and Behavior (six weeks), followed by 11 weeks of summer vacation starting in late May.
Year 1 course descriptions
All course-level objectives are derived from specific objectives within one of seven ACGME competencies. These objectives are referenced in parentheses in each course description.
Review all competencies and learning objectives
Students begin to appreciate their role as health care professionals by learning skills and attributes necessary to begin patient care as a novice member of a health care team.
Course objectives
-
Examine personal values and biases as well as professional goals and responsibilities. (P1)
-
Explore and apply ethical and legal principles that guide the practice of medicine. (P3)
-
Explain how both individual and systemic barriers contribute to disparities in healthcare delivery. (SBP3)
-
Explain the importance of and describe physician responsibility for patient safety. (SBP5)
-
Describe the roles and responsibilities of members of the healthcare team. (SBP6)
-
Demonstrate effective communication and collaboration skills in a team environment. (ISC1)
-
Identify one’s communication style and describe elements of and barriers to effective communication. (ISC3)
-
Describe strength and credibility of medical information sources. (PBLI3)
-
Apply principles of evidence-based medicine and biostatistics to form answerable clinical questions, analyze study design, interpret study findings, and evaluate diagnostic and therapeutic options. (MK5)
Students advance their clinical skills, knowledge and communication skills to acknowledge the social context of health and disease.
Course objectives
-
Demonstrate the essentials of taking a comprehensive patient history and perform a complete physical examination. (PC2)
-
Perform a problem-focused physical exam incorporating specific skills such as the appropriate use of an ophthalmoscope and otoscope and demonstrating the proper approach to specialized exams. (PC2)
-
Review a patient’s previous medical records to gather information as an adjunct to the data gathered in the clinical encounter. (PC2)
-
Begin to interpret diagnostic tests using foundational science knowledge. (PC4)
-
Within the context of patient encounters and patient care, analyze how an individual’s values, life circumstances, and familial and cultural influences can motivate his or her behavior, health care utilization, and interpretations of health care information and decision-making. (SBP3)
-
Students will be able to describe the impact of local, state, and federal policies and resources on individual and community health outcomes. (SPB4)
-
Analyze the organization, financing including principles of cost-effective care, and delivery of health care. (SPB4)
-
Demonstrate an awareness of the roles and responsibilities of the different members of the healthcare team. (SPB6)
-
Construct collaborative patient-centered decisions with other health professionals. (ISC1)
-
Demonstrate effective communication skills that permit an accurate and respectful gathering of information from patients. (ISC2)
-
Identify and demonstrate techniques for modifying communication that is sensitive to the differences, values, and needs of others, with attention to the context and purpose of the conversation. (ISC3)
-
Recognize techniques that contribute to shared decision making between physicians, patients and/or families. (ISC4)
-
Perform a basic oral presentation of patient history, physical exam, and problem summary for patient encounters. (ISC5)
-
Prepare a basic written documentation of patient history, physical exam, and problem summary for patient encounters. (ISC5)
-
Recognize the utility, benefits and limitations of an electronic health record. (ISC5)
-
Apply basic principles of evidence-based medicine: formulating a clinical question; searching and retrieving medical information from various evidence-based sources. (PBLI3)
-
Identify ethical issues and acknowledge their own moral value and the impact of this on patient care. (P1)
-
Identify unethical and unprofessional behaviors in others and begins to address these behaviors through conflict resolution or formal organizational/institutional channels (P4)
-
Recognize professional behavior and perform in a manner that is consistent with the medical profession’s accepted standards. (P2)
-
Adhere to ethical and legal principles that govern medical practice and medical documentation including patient confidentiality. (P4)
Medical students engage with health systems science topics using discussions, journal-clubs, guided reflections, and interprofessional education opportunities.
Course Objectives
-
Engage in self-directed learning by identifying individual knowledge and performance gaps and evaluating resources to improve performance. (PBLI1)
-
Provide and accept constructive feedback and engage in reflective practices. (PBLI3)
-
Articulate how self-awareness impacts patient care and individual well-being. (PBLI4)
-
Demonstrate effective communication skills and respectful dialogue during group discussion. (ICS1)
-
Identify and analyze difficult choices in biomedical ethics situations. (P3)
-
Define the roles and responsibilities of the different members of the healthcare team. (SBP1)
-
Identify social and structural determinants of health and describe their impact on individuals, populations, and health. (SBP2, HEAL2)
-
Describe relevant policies and finance models that inform health care decision making. (SBP3)
-
Describe principles of health care quality improvement. (SBP4)
-
Describe the principles of cost-effective care and the role of a physician in delivery of high-quality health care. (SBP5)
-
Apply principles of evidence-based medicine (EBM), scientific method and epidemiology to critically appraise medical literature. (MK5, MK6, MK7)
-
Discuss how systems of inequity have impacted marginalized communities and identify strategies to eliminate barriers to health equity. (HEAL1)
-
Identify opportunities for advocacy at the individual, group and population levels to improve health systems for patients. (HEAL3)
-
Describe the learned leadership traits and styles conducive to working in an interprofessional team. (HEAL3, SBP1)
Students’ knowledge of the functional and developmental relationship between anatomical structures, organs and organ systems enable them to explain the anatomic (microscopic and macroscopic) basis of common clinical conditions, injuries, diseases and functional deficits.
Course objectives
-
Describe the embryology of organ systems and the developmental abnormalities that lead to common congenital defects. (MK1)
-
Demonstrate knowledge of the structural and functional organization of the adult human body and its variations as visualized by direct dissection of human cadavers and by medical imaging techniques. (MK1)
-
Identify the histology and electron microscopic morphology of tissues and organs through the use of light and electron microscopy and discuss the functional aspects of the identified tissues. (MK1)
-
Demonstrate professionalism through respect for the donor, the medical education process, and their peers. (P2)
-
Identify gaps in their understanding of the developmental, histologic, and gross anatomic structure of the human body; locate, analyze and appraise information to overcome their knowledge deficits; and integrate new information to broaden their foundation of medical knowledge. (PBLI1)
Students’ knowledge of fundamental concepts in molecular, cell and tissue biology and in clinical genetics will enable them to explain the molecular, biochemical and cellular underpinnings of health and various disease states.
Course objectives
-
Describe the subcellular structure of mammalian cells, the function of the different subcellular organelles, including cell membranes and associated proteins, and their relevance to human health and disease. (MK1)
-
Describe how cells divide, differentiate, control their shapes and activities to produce basic tissue types and explain how their microscopic characteristics produce the functions of these tissues and their specialized subtypes. (MK1)
-
Describe the molecular and cellular events of human development from fertilization through formation of the notochord and body plan, including the molecular basis of various developmental abnormalities and methods for their detection. (MK1)
-
Use knowledge of protein structure, folding and assembly, including the role of co-factors, to explain how altered protein structure can have pathological consequences. (MK1)
-
Describe how protein function is regulated and how dysregulation contributes to human disease. (MK1)
-
Describe the organization, function, maintenance, and regulation of the human genome; explain how these processes or their dysfunction contribute to health and disease at the individual, family and population levels, and apply genetic methods for calculating/assessing risk of disease occurrence. (MK1)
-
Describe how the evolving insight into the molecular basis of disease affects ethical considerations in the diagnosis and treatment of disease (P3).
-
Describe how the metabolism of carbohydrates, lipids, nucleotides, and proteins generate the energy and intermediates necessary for cell and organ homeostasis and how dysregulation of these processes (inborn and acquired) contributes to human disease. (MK1)
-
Distinguish the various mechanisms of cell-to-cell communication and describe how dysfunction in these processes contributes to human disease. (MK1)
-
Describe the genetic, molecular and cellular events and the environmental factors linked to the initiation, progression, and metastasis of cancers and describe how these elements may impact risk assessment and point to targets for therapeutic intervention, prevention, and/or risk reduction for particular types of cancer. (MK1)
-
Identify gaps in their understanding of cell and molecular biology; locate, analyze and appraise information required to fill those gaps; and integrate new information to extend medical knowledge. (PBLI1)
-
Behave in a professional manner by demonstrating compassion, honesty, integrity, respect, responsibility, and self-discipline in relationships with all individuals, regardless of gender, age, culture, race, ethnicity, religion, sexual orientation, disability, socioeconomic status, native language or role. (P2)
-
Modify communications demonstrating sensitivity to differences, values, and needs of others, with attention to one’s personal communication style and the context and purpose of the conversation. (ISC3)
-
Share information accurately in academic and clinical settings both in oral presentations and written documentation including in the medical record. (ISC5)
Students’ knowledge of physiological, pathophysiological and pharmacological principals enable them to describe maintenance of normal physiologic functions and discuss disease states and drug treatments in terms of altered cellular and tissue function.
Course objectives
-
Explain the fundamental physiological functions of the cardiovascular, pulmonary and renal systems and explain their roles in contributing to homeostasis of the body, including neurohumoral control mechanisms. (MK1)
-
Explain fundamental mechanisms of cellular and tissue responses to injury and disease. (MK3)
-
Describe how the physical environment influences health and disease. (MK2)
-
Explain the general pathophysiology of neoplastic tumors, including the progression of tumor growth, clinical consequences, and the mode of action of representative antineoplastic therapies. (MK3)
-
Describe basic pharmacokinetic principles of drug absorption, distribution, biotransformation and excretion and utilize this knowledge to explain pharmacodynamic actions, and interactions of commonly prescribed drugs. (MK4)
-
Identify gaps in personal knowledge when presented with new clinical scenarios and integrate basic science principles to explain and interpret the clinical features of the case. (PBLI2)
-
Given a specific disease state, explain how alterations of tissue structure and function contribute to the clinical consequences of the disease and describe appropriate therapeutic approaches. (MK4)
-
Given a clinical problem, generate a personal learning objective to address a gap in knowledge, use multiple resources to address the question, and use principles of evidence-based medicine to assess the quality of resources and interpret the information. (PBLI3)
-
Modify communications demonstrating sensitivity to differences, values, and needs of others, with attention to one’s personal communication style and the context and purpose of the conversation or presentation. (ISC3)
-
Share information accurately in academic and clinical settings both in oral presentations and written documentation including in the medical record. (ISC5)
Students’ knowledge of the immune system and the pathogenesis of infectious organisms enable them to formulate appropriate diagnostic and interventional strategies for the prevention and treatment of infectious diseases and immune-mediated pathologies.
Course objectives
-
Explain the development, structure, function and regulation of the immune system at molecular and cellular levels, and differentiate between the innate and adaptive mechanisms of host defense against microbial pathogens. (MK1)
-
Describe the structure, physiology, genetics, pathogenesis and epidemiology of the major classes of infectious organisms associated with human diseases. (MK2)
-
Differentiate among the major pathogens associated with gastrointestinal, respiratory, CNS, skin and soft tissue, bone, circulatory, and urogenital infections, and illustrate how host defense mechanisms, diagnostic strategies, and therapeutic approaches differ between organ systems. (MK3)
-
Describe the key characteristics of primary and acquired immunodeficiencies, analyze their clinical consequences, and define infectious organisms associated with these disorders. (MK2)
-
Illustrate the basic principles of immunization. (MK4)
-
Explain the mechanisms of action of the major classes of antibiotics, anti-virals, anti-fungals, and anti-parasitic agents, including their use against specific pathogens, their effect on normal flora, adverse reactions, and the problem of drug resistance. (MK4)
-
Identify and explain the pathophysiology of allergies and other hypersensitivities, autoimmunity, transplantation, and immune responses to cancer. (MK2)
-
Categorize methods to prevent the spread of contagious organisms, including universal precautions, sterile techniques, sterilization, and disinfection, and apply these methods to the prevention of foodborne diseases and nosocomial infections. (MK6)
-
Explain how issues of geography, economics, culture, and public health affect patterns of infectious diseases epidemiology and approaches to disease prevention. (MK6)
-
Identify gaps in your understanding of Host Defense, identify and evaluate resources to help close these gaps, and articulate the information to your peers. (PBLI1)
-
Behave in a professional manner and carry out any responsibilities in Host Defense with the highest levels of integrity. (P2)
Students’ knowledge of the physiology, pathophysiology and pharmacology of the brain and the nervous system and their knowledge of mind-body interactions enable them to describe the major diseases of these systems, including their signs and symptoms, behavioral patterns, histopathologic and clinical laboratory characteristics, and rationale for current therapeutic interventions.
Course objectives
-
Describe the gross, histologic, and cellular structure of the central and peripheral nervous system. (MK1)
-
Describe the anatomic connectivity and physiologic processes underlying the major functional systems (motor, sensory, homeostatic, and higher cortical functions) of the nervous system. (MK1)
-
Localize lesions of the peripheral and central nervous system by recognizing patterns of neurologic deficits from the patient history and neurologic exam (MK2)
-
Recognize the clinical presentations of major diseases of the nervous system and describe how the neurologic exam, mental status exam, and common diagnostic tests and procedures are used to develop a differential diagnosis for diseases of the nervous system. (MK3)
-
Describe the pharmacological therapies (including drug class, mechanism of action, adverse effects, contraindications, drug-drug interactions, and pharmacokinetics), surgical approaches, and prosthetic devices for the treatment and management of common nervous system disorders. (MK4)
-
Describe how sensory, cognitive and environmental factors interact in the experience of neurologic and psychiatric symptoms, and how psychosocial and behavioral interventions can be used to promote health and treat disease. (MK7)
-
Describe the neurologic and psychiatric symptoms associated with drugs of abuse, the underlying mechanisms of dependence, withdrawal, and addiction, and treatment strategies. (MK2)
-
Describe the normal development of the nervous system, structural and clinical manifestations of common congenital anomalies, and the impact of genetic and environmental factors on fetal development and behavior in the pediatric and adult population. (MK1)
-
Demonstrate proficiency in self-directed and life-long learning skills through the gathering, analysis, synthesis, evaluation and communication to peers of new information that the student self-identifies as necessary to understand more completely the causes, effects and treatments of neurological problems (PBLI3)
-
Behave in a professional manner by demonstrating compassion, honesty, integrity, respect, responsibility, and self-discipline in relationships with all individuals, regardless of gender, age, culture, race, ethnicity, religion, sexual orientation, disability, socioeconomic status, native language or role. (P2)
-
Modify communications demonstrating sensitivity to differences, values, and needs of others, with attention to one’s personal communication style and the context and purpose of the conversation (ISC3)
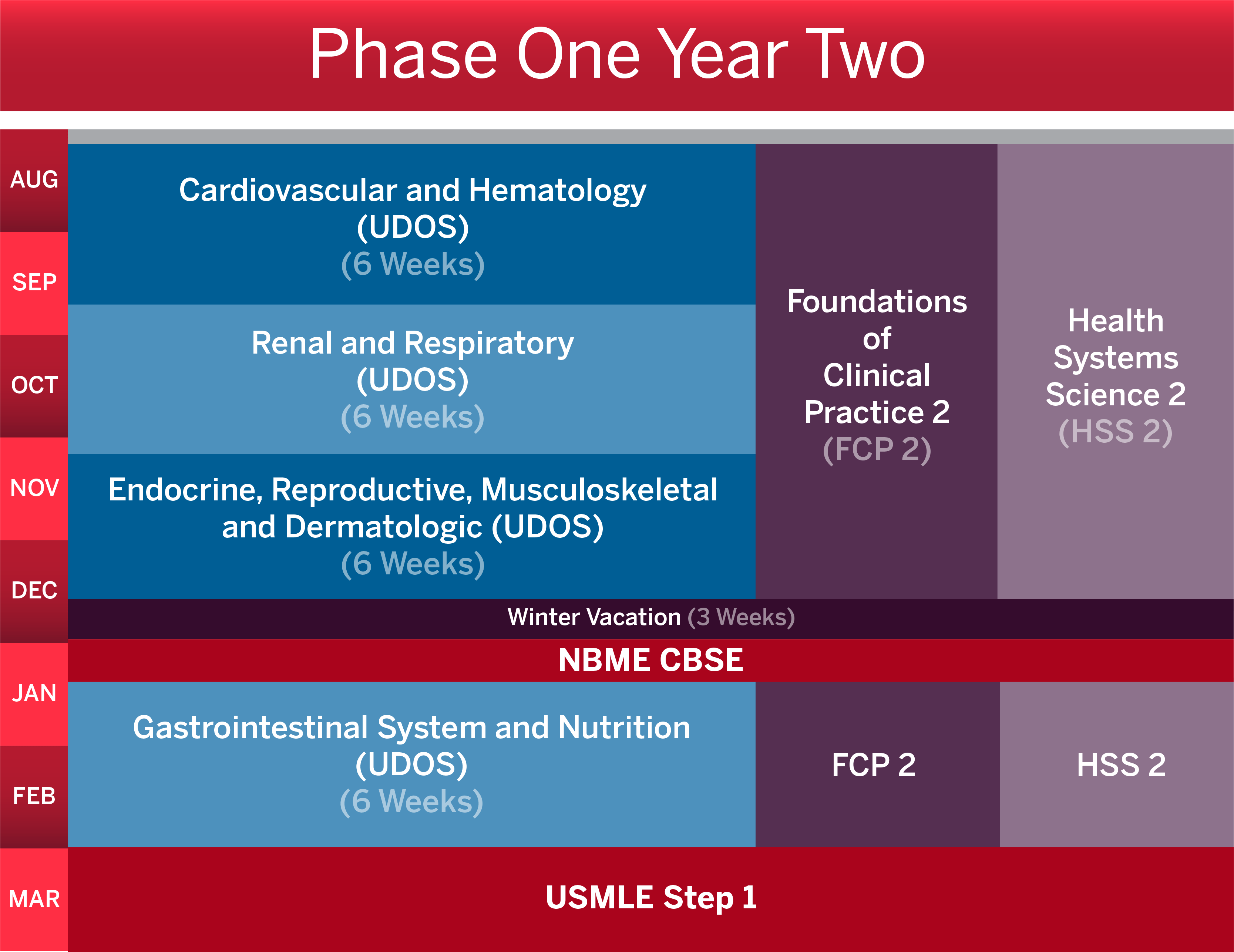
Beginning in August, the Cardiovascular and Hematology course runs for six weeks. In mid-September, the Renal and Respiratory course begins and also last for six weeks. The Gastrointestinal System and Nutrition course begins in early November and runs for six weeks.
Foundations of Clinical Practice 2 and Health Systems Science 2 courses both run from August through December.
In mid-December, students have a three week winter vacation followed by time for the National Board of Medical Examiners (NBME) Comprehensive Basic Science Examination (CBSE). In mid-January, students take the Endocrine, Reproductive, Musculoskeletal and Dermatologic course for six weeks. They also continue in Foundations of Clinical Practice 2 and Health Systems Science 2.
In March, students have protected time for United States Medical Licensing Exam (USMLE) Step 1.
Year 2 course descriptions
All course-level objectives are derived from specific objectives within one of seven ACGME competencies. These objectives are referenced in parentheses in each course description.
Review all competencies and learning objectives
Students advance their clinical skills, knowledge and communication skills acknowledging the social context of health and disease
Course objectives
-
Within the context of patient encounters and patient care, analyze how an individual’s values, life circumstances, and familial and cultural influences can motivate his or her behavior, health care utilization, and interpretations of health care information and decision-making. (SBP2)
-
Recognize techniques that contribute to shared decision making between physicians, patients and/or families. (ISC4)
-
Demonstrate the essentials of taking a comprehensive patient history and perform a complete physical examination. (PC1)
-
Demonstrate effective communication skills that permit an accurate and respectful gathering of information from patients. (ISC2)
-
Generate appropriate differential diagnoses for a variety of patient presentations and begin to select appropriate diagnostic tests and interpret results with respect to the presumptive pathophysiological disease process. (PC2)
-
Begin to interpret diagnostic tests using foundational science knowledge. (PC3)
-
Perform a basic oral presentation of patient history, physical exam, problem summary and differential diagnosis for patient encounters. (ISC5)
-
Prepare a basic written documentation of patient history, physical exam, problem summary and differential diagnosis for patient encounters. (ISC5)
-
Apply basic principles of evidence-based medicine: formulating a clinical question; searching and retrieving medical information from various evidence-based sources. (PBLI1)
-
Identify ethical issues and acknowledge their own moral value and the impact of this on patient care. (P1)
-
Identify unethical and unprofessional behaviors in others and begins to address these behaviors through conflict resolution or formal organizational/institutional channels (P3)
-
Demonstrate an awareness of the roles and responsibilities of the different members of the healthcare team (SBP1)
-
Recognize professional behavior and perform in a manner that is consistent with the medical profession’s accepted standards. (P2)
-
Demonstrate the ability to take a problem-focused history from a patient, obtaining necessary information in an efficient manner. (PC1)
-
Identify and demonstrate techniques for modifying communication that is sensitive to the differences, values, and needs of others, with attention to the context and purpose of the conversation. (ISC3)
-
Perform a problem-focused physical exam incorporating specific skills such as the appropriate use of an ophthalmoscope and otoscope and demonstrating the proper approach to specialized exams such as the neurologic exam and exam of the genitalia and joints. (PC1)
-
Review a patient’s previous medical records to gather information as an adjunct to the data gathered in the clinical encounter. (PC2)
-
Recognize the utility, benefits and limitations of an electronic health record. (ISC5)
-
Construct collaborative patient-centered decisions with other health professionals. (ISC1)
-
Identify adherence to preventative medicine. (SBP2)
-
Describe the impact of local, state, and federal policies and resources on individual and community health outcomes. (SPB3)
-
Adhere to ethical and legal principles that govern medical practice and medical documentation including patient confidentiality. (P3)
-
Analyze the organization, financing including principles of cost-effective care, and delivery of health care. (SBP5)
Medical students engage with health systems science topics using discussions, journal-clubs, guided reflections, and interprofessional education opportunities.
Course objectives
-
Engage in self-directed learning by identifying individual knowledge and performance gaps and evaluating resources to improve performance. (PBLI1)
-
Provide and accept constructive feedback and engage in reflective practices. (PBLI3)
-
Articulate how self-awareness impacts patient care and individual well-being. (PBLI4)
-
Demonstrate effective communication skills and respectful dialogue during group discussion. (ICS1)
-
Identify and analyze difficult choices in biomedical ethics situations. (P3)
-
Define the roles and responsibilities of the different members of the healthcare team. (SBP1)
-
Identify social and structural determinants of health and describe their impact on individuals, populations, and health. (SBP2, HEAL2)
-
Describe relevant policies and finance models that inform health care decision making. (SBP3)
-
Describe principles of health care quality improvement. (SBP4)
-
Describe the principles of cost-effective care and the role of a physician in delivery of high-quality health care. (SBP5)
-
Apply principles of evidence-based medicine (EBM), scientific method and epidemiology to critically appraise medical literature. (MK5, MK6, MK7)
-
Discuss how systems of inequity have impacted marginalized communities and identify strategies to eliminate barriers to health equity. (HEAL1)
-
Identify opportunities for advocacy at the individual, group and population levels to improve health systems for patients. (HEAL3)
-
Describe the learned leadership traits and styles conducive to working in an interprofessional team. (HEAL3, SBP1)
Students’ knowledge of the physiology, pathophysiology and pharmacology of the cardiovascular and hematologic systems enable them to describe the major diseases of these systems, including their signs and symptoms, histopathologic and clinical laboratory characteristics, and rationale for current therapeutic interventions.
Course objectives
-
Describe hematopoiesis, explain how it is controlled, and recognize the consequences of dysfunction. (MK1)
-
Describe the coagulation system, explain how it is controlled, and recognize how perturbations of this system leads to disease. (MK1)
-
Define blood types, describe the common clinical laboratory assessments used for hematologic function, recognize abnormal values, and interpret significance. (MK3)
-
Apply blood banking principles to select appropriate transfusion therapies, and recognize adverse outcomes. (MK4)
-
Describe and categorize common therapeutic modalities for hematologic disorders and malignancies, and explain their mechanisms. (MK4)
-
Classify and differentiate hematologic malignancies, including pathophysiology, presentation, and diagnostics. (MK3)
-
Explain the manifestations of functional and structural heart diseases and the pathophysiologic mechanisms and functional consequences of these disorders. (MK3)
-
Explain the manifestations of major vascular diseases and the pathophysiologic mechanisms and functional consequences of these disorders. (MK3)
-
Explain the mechanisms and consequences of myocardial ischemia, arrhythmias, sudden death, and different classifications of cardiovascular collapse (shock). (MK3)
-
Recognize the classic sentinel cardiovascular presentations, explain their pathophysiologic mechanisms, and the mechanisms that underlie the utilization of diagnostic tools for cardiovascular disease screening and diagnosis. (MK3)
-
Explain the mechanisms and applications for the common therapeutic modalities utilized in the management of cardiovascular disorders. (MK4)
-
Describe the development of psychiatric issues related to diagnosis of serious or life-long medical conditions, explain how they can adversely affect treatment and patient adherence, recognize the consequences of patient and caregiver stress and dysfunction, and demonstrate the ability to communicate the difference between healing and curing. (MK7)
-
Describe the impact of culture and ethnicity, gender and socioeconomic status on prevalence, prevention, diagnosis and intervention, recognize and explain how limited or absent resources can negatively impact treatment options, patient adherence, recovery, and cause consequences for the family and caregivers. (SBP2)
-
Given clinical questions in cardiovascular and hematology, generate and analyze a set of potential solutions by applying prior knowledge to a new experience, recognizing the limitations of prior experience and knowledge, and identifying new information required to solve the problem. (PBLI1)
-
Given clinical scenarios in cardiovascular and hematology, demonstrate an awareness of the roles and responsibilities of the different members of the health care team including complex multidisciplinary care and regional care systems. (SBP1)
-
Apply the concept of high value care to diagnostic and therapeutic clinical scenarios of patients with hematologic or cardiovascular disease. (SBP5)
Students’ knowledge of the physiology, pharmacology and pathophysiology of the respiratory and renal systems enable them to describe the major diseases of these systems, including their signs and symptoms, histopathologic and clinical laboratory characteristics, and rationale for current therapeutic interventions.
Course objectives
-
Describe the purpose, function, and regulation of the respiratory and renal systems using relevant anatomical and biochemical parameters. (MK1)
-
Explain the pathophysiological basis of respiratory, renal, and urinary diseases through analysis of anatomic, histological and biochemical alterations of system function. (MK2)
-
Evaluate clinical presentations and formulate appropriate respiratory, renal, and urinary disease differentials through assessment of patient history, physical exam and diagnostic testing. (MK3)
-
Apply pharmacologic, mechanistic, and behavioral therapies to counteract or prevent pathophysiologic mechanisms causing respiratory, renal, and urinary diseases. (MK4)
-
Employ the principles of evidence-based medicine to evaluate the efficacy of diagnostic and therapeutic options in patients with respiratory, renal, and urinary disorders. (MK5)
-
Describe the epidemiology of common respiratory, renal, and urinary diseases, the methods for prevention and early detection of these diseases, and systematic, population-based approaches for reducing the incidence and prevalence of disease. (MK6)
-
Explain how behavioral, cultural, economic, educational, environmental, lifestyle, and psychosocial factors impact the renal and respiratory health of patients and the effect of care seeking, care compliance, barriers to care, and attitudes towards care. (MK7)
-
Recognize ethical and professional responsibilities in caring for patients with respiratory or renal system failure and critically examine the implications of physician bias and self-awareness. (P3)
-
Demonstrate self-directed and life-long learning skills through: identification of learning needs, gathering relevant information from multiple sources, analyzing the quality and relevance of this information, and synthesizing the information to apply and communicate to colleagues. (PBLI1)
-
Establish and maintain respectful relationships with peers, faculty, and staff to foster an effective learning environment. (ISC1)
Students’ knowledge of the physiology, pathophysiology and pharmacology of the gastrointestinal system enable them to describe the major diseases of this system, including their signs and symptoms, histopathologic and clinical laboratory characteristics, and rationale for current therapeutic interventions including the application of principles of nutrition and their role in health and disease.
Course objectives
-
Describe the function of gastrointestinal organs and tissues with emphasis on how their functions relate to their structure, and how they are regulated. (MK1)
Explain etiology of certain gastrointestinal diseases including the molecular and genetic mechanisms underlying the diseases. (MK2) -
Recognize the major diseases of the gastrointestinal system and discuss their pathophysiology; explain how pathophysiologic mechanisms result in characteristic anatomic, histologic, imaging, and laboratory features of particular diseases. (MK3)
-
Describe the clinical signs and symptoms of gastrointestinal and nutritional diseases and how they guide diagnosis. (MK3)
-
Explain the indications for and mechanism of action of drugs and procedures used to treat gastrointestinal diseases. (MK4)
-
Apply case-based medical problem-solving using clinical and scientific resources to identify gaps in knowledge related to gastrointestinal conditions. (PBLI1)
-
Explain the impact of nutritional intake on health and disease in adults and children recognize how health status can impact nutritional requirements (MK1)
-
Describe how nutritional interventions can be used to promote health and to treat disease (MK4)
-
Recognize psychosocial aspects of gastrointestinal and nutritional disorders and evaluate the importance of a patient’s social context in health and disease and how factors such as culture, socio-economic status, environment, religion, spirituality, education, and health literacy impact nutrition and associated health outcomes. (MK7)
Students’ knowledge of the physiology, pathophysiology, and pharmacology of dermatologic and musculoskeletal systems enable them to describe the major diseases of these systems, including their signs and symptoms, histopathologic and clinical laboratory characteristics, and rationale for current therapeutic interventions.
Students’ knowledge of the physiology, pathophysiology and pharmacology of the endocrine and reproductive systems enable them to describe the major diseases of these systems, including their signs and symptoms, histopathologic and clinical laboratory characteristics, and rationale for current therapeutic interventions.
Course objectives
-
Explain the function of the endocrine, reproductive, musculoskeletal and dermatologic organs and tissues with emphasis on how their functions relate to their structure and how their activity is regulated across the lifespan. (MK1)
-
Recognize major diseases of the endocrine, reproductive, musculoskeletal and dermatologic systems based on pathophysiologic mechanisms, genetic predispositions, and their interrelationships. (MK3)
-
Describe how pathophysiologic mechanisms result in characteristic anatomic, histological, laboratory and clinical presentations of a particular disease. (MK3)
-
Formulate a differential diagnosis based on the integration of clinical, biochemical, pathologic and radiographic data. (MK3)
-
Explain the mechanism of action and potential side effects of drugs, devices, and interventions used to treat the diseases of the endocrine, reproductive, musculoskeletal and dermatologic systems based on knowledge of the pathophysiology. (MK4)
-
Describe how psychosocial and behavioral interventions can be used to promote endocrine, reproductive, musculoskeletal and dermatologic health. (MK4)
-
Describe the epidemiology of endocrine, reproductive, musculoskeletal and dermatologic system disorders. (MK7)
-
Identify personal and scientific knowledge gaps in the diagnosis and management of endocrine, reproductive, musculoskeletal and dermatologic conditions, and investigate resources to address these deficiencies. (PBLI2)
-
Apply foundational principles of medical ethics to identify and address ethical issues surrounding issues in medical therapy and research. (P3)
-
Analyze the economic and psychosocial impact of chronic musculoskeletal and skin disease on the individual and community. (SBP2)