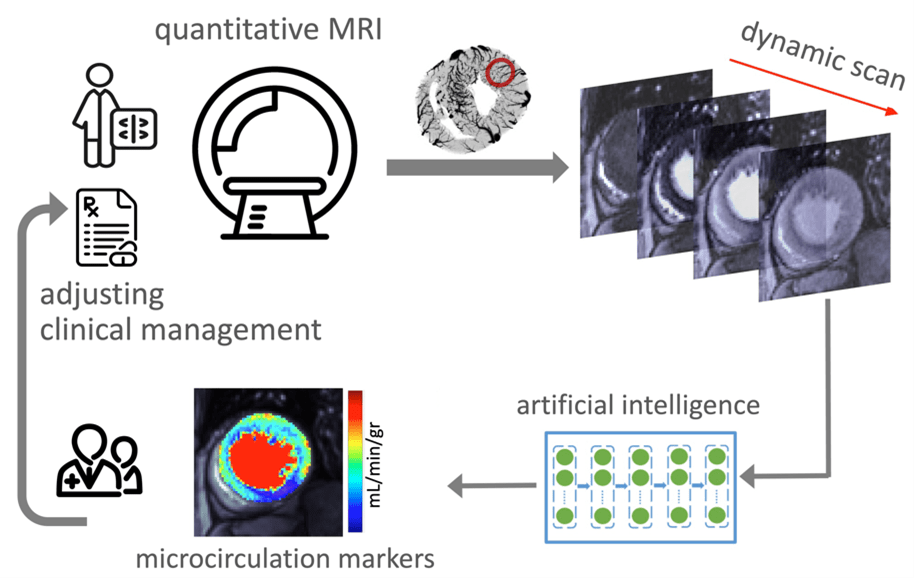
Microcirculation refers to the network of small vessels that supply oxygen-rich blood to the surrounding tissue. Patients with signs and symptoms of cardiovascular disease may suffer from microvascular disease, that is, the dysfunction of microcirculation in their heart muscle, which in turn, represents an important target for established or novel medical therapies. KCVRC scientists develop cutting-edge translational magnetic resonance imaging (MRI) techniques to investigate coronary microvascular function and to discover new markers that track the health of coronary microcirculation and quantify its response to therapy.

Improving the clinical paradigm for assessing endotypes of microvascular dysfunction
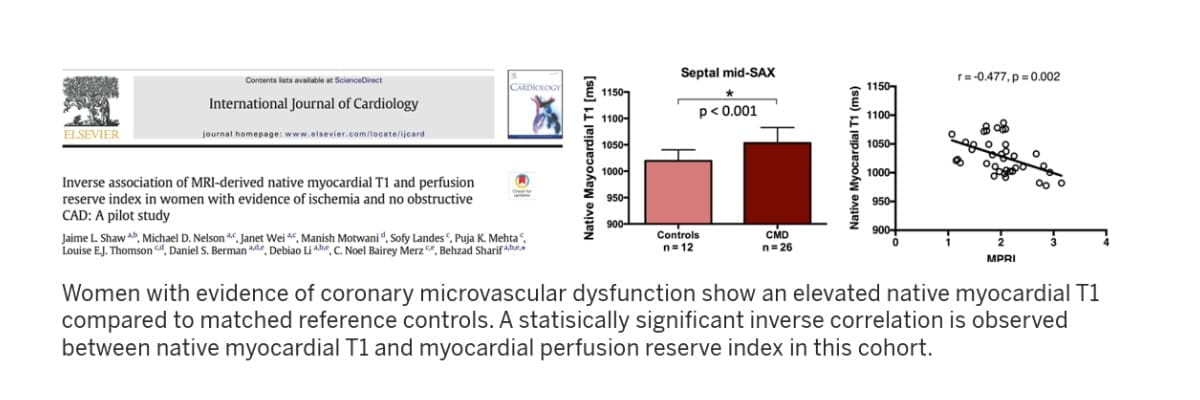
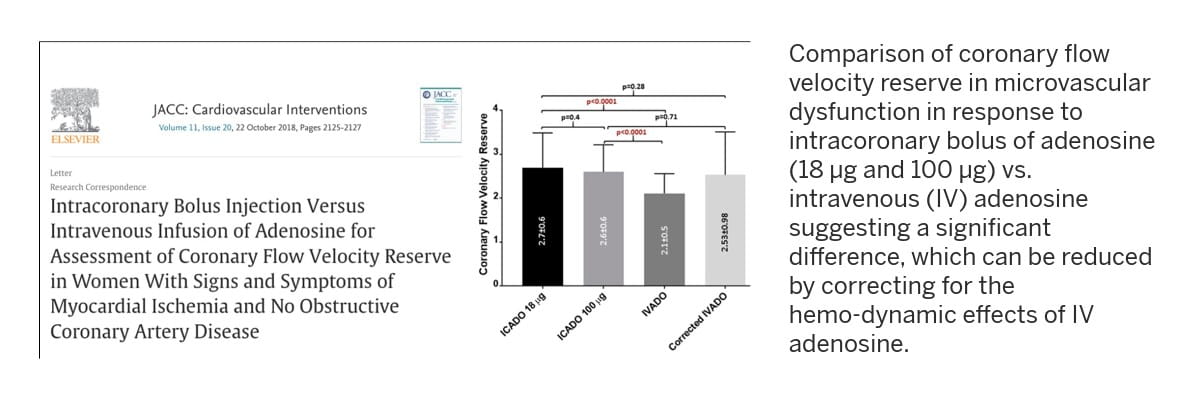
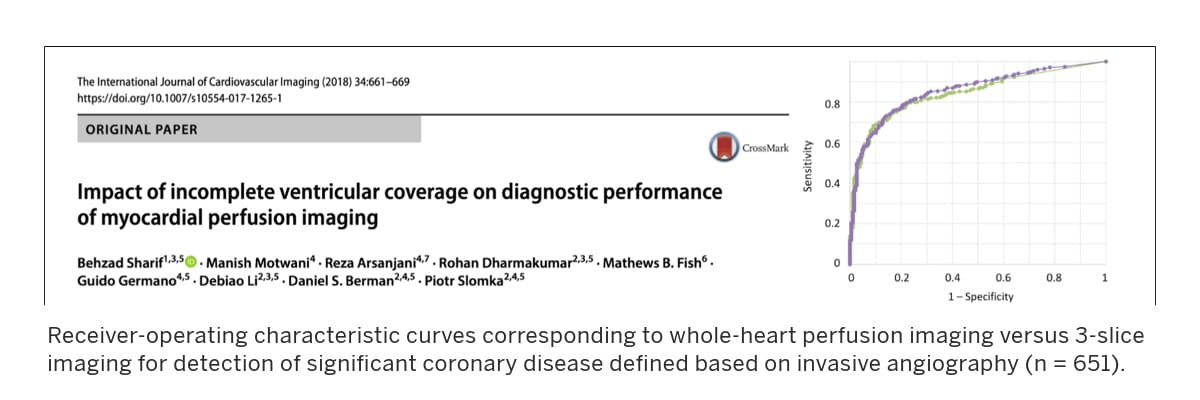
Led by Behzad Sharif, PhD, KCVRC investigators within the Microcirculaton Research program are advancing new approaches for noninvasive and minimally invasive assessment of patients with microvascular dysfunction by developing MRI-based techniques to quantify various markers of coronary microcirculation.
Two approaches advance the diagnosis and clinical management of patients affected by microvascular disease:
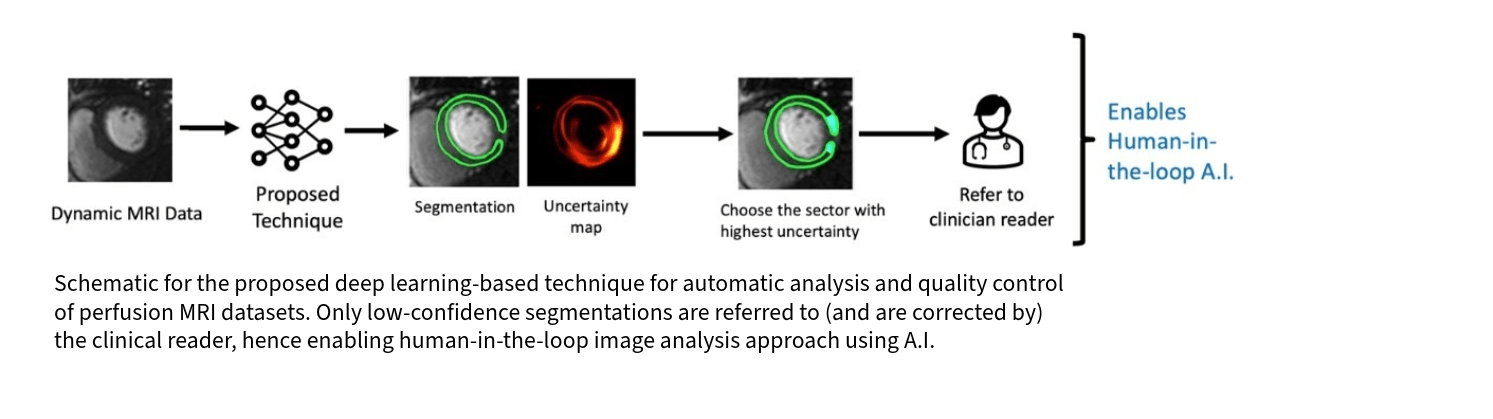
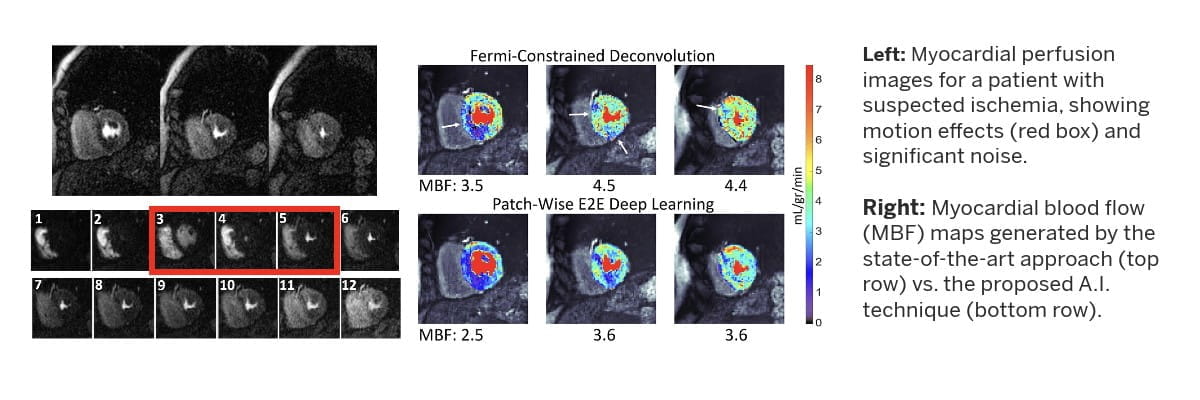
- Reliable noninvasive assessment of microvascular health and function, including discovery and validation of new functional MRI markers of tissue microcirculation by leveraging multi-disciplinary innovations in magnetic resonance physics, computational engineering and machine learning
- Development and validation of new interventional MRI approaches, enabling minimally invasive testing and endotype detection for microvascular disease, structural heart disease and cardiometabolic disorders.
A significant component of our research effort is devoted to developing artificial intelligence-enabled MRI strategies (pulse sequences and accelerated image formation) and computational image analysis techniques aimed at enabling accurate characterization of the relationship between imaging markers of microcirculation and progression of disease, or response to therapy, in the context of nonobstructive coronary artery disease and cardiometabolic disorders.
Research in this lab is supported by the NIH National Heart, Lung and Blood Institute and the Lilly Endowment through the INCITE program.