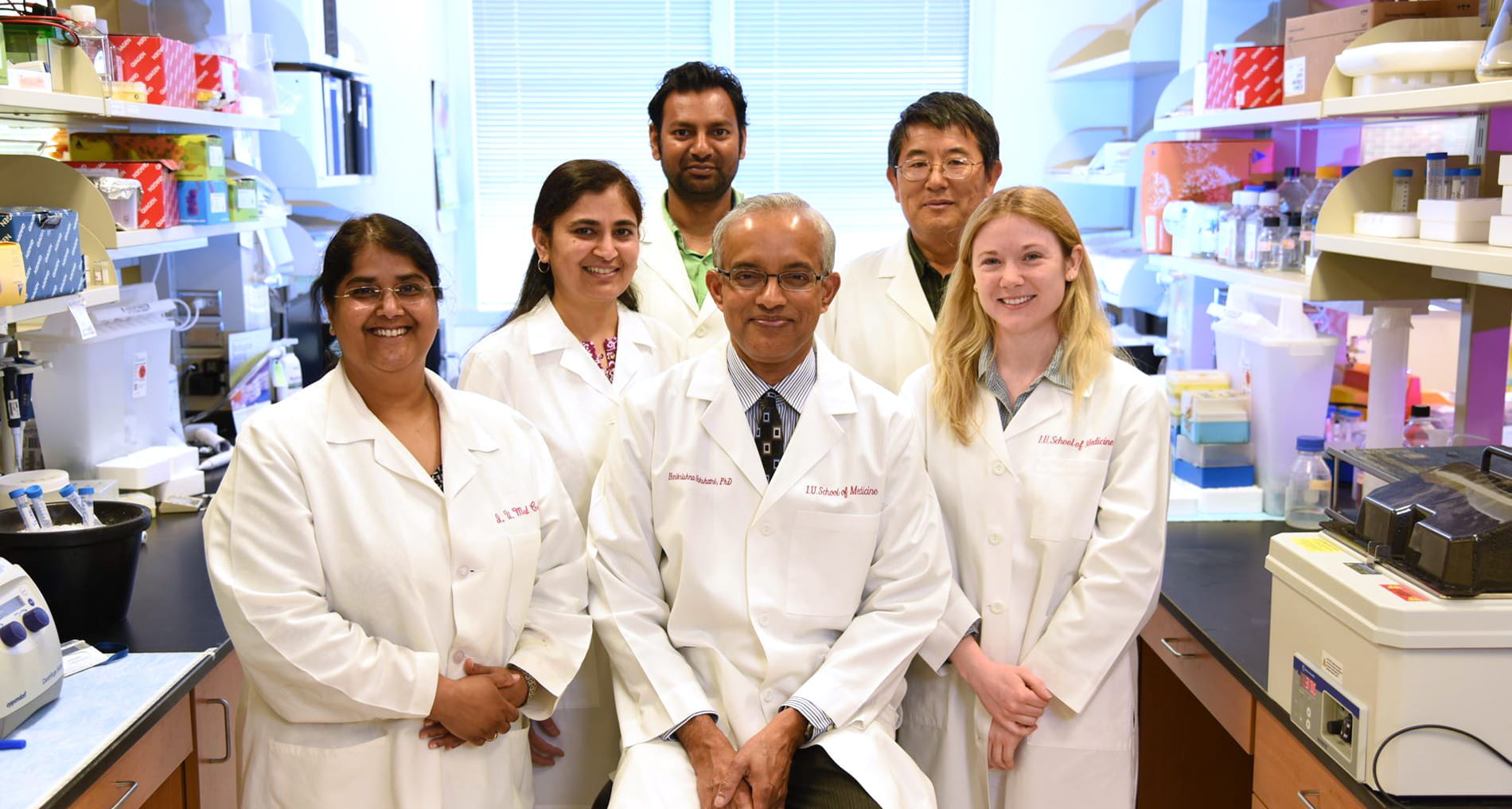
The Surgical Outcomes & Quality Improvement Center (SOQIC), is a nationally recognized research hub focused on improving health care quality across surgical specialties, supported by over $40 million in funding. With work published in top journals like JAMA and NEJM, SOQIC also trains medical students, residents and fellows through robust, grant-supported programs. SOQIC offers a multidisciplinary two-year research training program for surgical residents, providing experience across surgical outcomes, health services, quality improvement, implementation science, health policy and education, with funded positions including the NIH NCI T32 in surgical oncology, Surgical Education Numbered Trials Fellowship, ACS Cancer Programs Fellowship, ASMBS Research Collaborative Fellowship and SAGES Fellowship.
Surgical Research Reimagined