Lab-grown organoids could be powerful tool for eye disease research, drug discovery
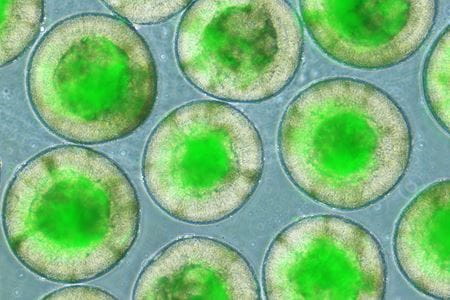
INDIANAPOLIS — Indiana University School of Medicine researchers have designed a quicker and more consistent way to grow mini models of the human retina in a lab.
Recently published in PNAS, their findings greatly standardize and streamline the process of creating these "mini retinas," also known as retinal organoids, which could accelerate eye research and help scientists better understand eye diseases and how to treat them.
"The ability to take stem cells derived from human donors and then generate retinal tissue from them provides us with a very powerful approach to studying how the human retina develops," said Jason S. Meyer, PhD, senior author of the study and associate professor of medical and molecular genetics and the A. Donald Merritt Investigator of Medical and Molecular Genetics at the IU School of Medicine. "Further, when these cells have a genetic basis for retinal disease, retinas grown in a dish can be used to better understand the disease process itself and serve as a platform for drug discovery."
In the past, the process of producing retinal organoids was too inefficient or the resulting organoids were too inconsistent — different sizes, shapes and compositions — to use in such large-scale studies as would be required for things like drug screening, said Meyer, who is also director of the Cell Research Group within the school's Stark Neurosciences Research Institute.
"In this new study, we have achieved 100% efficiency of retinal organoid production across multiple donors, with each retinal organoid much more reproducible in their size and shape, facilitating comparative studies," he said.
How did they do it?
- Size matters: The scientists observed that when initial stem cell groupings were constructed with too few cells, they lost the ability to achieve the 100% purity of retinal organoids – demonstrating the importance of having the correct size (1000 cells per dish or more) of initial cellular clusters.
- Special signal: They also activated a special signaling pathway called Bone Morphogenetic Proteins (BMP), which is like unlocking a secret genetic code that tells the developing cells to become retinas.
- Timing is everything: Although prior studies had explored some of the factors that the current study found to be important to achieve high reproducibility in generating these retinal organoids, this new study demonstrated how critical it is to achieve precise timing of experimental manipulations to achieve highly reproducible mini retinas.
Jade Harkin, PhD, first author of the study and a recent PhD graduate of the IU School of Medicine, said the study's results are a "game-changer" for the future of eye research.
"The ability to generate more reproducible retinal organoids at 100% efficiency — meaning we get it right every time — will be beneficial for high-throughput R&D studies and will speed up the development of new therapies and drugs for retinal degenerative diseases," Harkin said.
Other authors of the study include IU School of Medicine's Kiersten H. Peña, Cátia Gomes, Melody Hernandez, Sailee S. Lavekar, Kaman So, Kelly Lentsch, Elyse M. Feder, Sarah Morrow, Kang-Chieh Huang, Kaylee D. Tutrow and Chi Zhang and the University of Kentucky's Ann Morris.
About the IU School of Medicine
The IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability. According to the Blue Ridge Institute for Medical Research, the IU School of Medicine ranks No. 13 in 2023 National Institutes of Health funding among all public medical schools in the country.
Writer: Andrea Zeek, anzeek@iu.edu
Sources: Jason Meyer, meyerjas@iu.edu, and Jade Harkin, harkinj@iu.edu
For more news, visit the IU School of Medicine Newsroom: medicine.iu.edu/news
Follow us on X: @IUMedSchool