As people across the United States are stocking up on groceries and staying home from work or school because of the COVID-19 crisis, faculty physicians and researchers from Indiana University School of Medicine are working to treat those infected and learn more about the virus.
“We are working together as best we can,” said W. Graham Carlos, MD, associate professor of clinical medicine at IU School of Medicine and chief of internal medicine at Eskenazi Health.
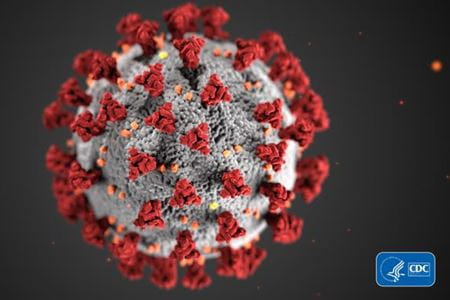
Now more commonly known as the coronavirus or COVID-19, SARS-CoV2 is a type of coronavirus thought to originate in China that is new to humans. The first known COVID-19 patient began feeling ill on December 10, 2019. In only four months, the highly contagious virus has spread to more than 350,000 known patients and resulted in more than 15,000 deaths worldwide—with those numbers climbing dramatically every day.
“The virus can infect the person for a period of days, maybe more, without the person knowing it,” Carlos said. “They can become contagious and spread it to other people, unbeknownst to anyone, before symptoms set in. It can spread rapidly and through communities, which is why we must stay away from each other by closing schools and community events at this time. That property in the virus makes it very dangerous in terms of its contagiousness.”
What makes this particular virus even more concerning is the way it is impacting people in vulnerable populations—most of those who have died were above age 65 or had an underlying condition like diabetes or lung disease.
How do we diagnose it?
For the most part, symptoms of COVID-19 include a fever, cough and shortness of breath. But some can have other symptoms as well, while others may never show symptoms. For reasons doctors don’t yet understand, children rarely show many symptoms, if any, but they can still carry the virus and spread it to others, including the elderly or those with underlying conditions who are more likely to experience severe cases. Because it can affect so many people so differently, it can be tricky to diagnose without an official test, which is a polymerase chain reaction (PCR) test completed off a nasal swab.
“Patients that have certain conditions, let's say emphysema, may feel shortness of breath more quickly, maybe even before they start to experience fever,” Carlos said. “Patients who have medical conditions or diseases that already have elements of coughing, like asthma or lung fibrosis, are going to be difficult to sort out, because it's hard for us to know without testing if this is an exacerbation of their typical known disease or if they've been infected with the coronavirus.”
More and more test kits are becoming available, which physicians say are important to learn how many cases of this virus truly exist in the community.
“Knowing who is positive gives a sense of how the population in each state is affected and what the spread is like, because it’s probably quite different for different states. If we know the people who are infected, we can more effectively isolate infected people and their contacts, and more rapidly contain the epidemic,” said Chandy John, MD, MS, Ryan White endowed professor of pediatrics and director of the Ryan White Center for Pediatric Infectious Disease and Global Health at IU School of Medicine and Riley Hospital for Children.
When the virus first hit the United States, John said there were only so many test kits available, and it could take days to get test results back from a lab. To keep up, practitioners have been prioritizing health care workers, who are at risk of contracting the virus from patients, and those most vulnerable to the virus, like patients with diabetes, lung suppression, heart disease, lung disease or kidney disease.
Thankfully, more institutions and health organizations are creating a supply of test kits, so John expects the number of tests administered each day to increase over time. As more testing occurs, more positive cases will be identified.
“I think there is going to be some level of concern or even panic over people thinking ‘Wow, all these people have COVID-19 now,’” John said. “But it’s not a cause for panic, because the increase is because of increased testing. A lot of people still question if we are overreacting or is this real. When you have testing, that gives more accurate numbers, people will know it’s real.”
But doctors also have a warning for those who may test negative for the virus.
“I’m concerned some people may think they have the virus, get the test, find out the test is negative, and then think they can become complacent and stop social distancing,” Carlos said. “If they're not careful, they may get the virus a couple of days after they've had a negative test.”
How do we treat it?
Because COVID-19 is new to humans and is spreading around the world rapidly, there hasn’t been enough time for researchers to heavily study the virus. But faculty at IU School of Medicine are utilizing data from cases in other countries and in the United States to learn more about it.
“Usually we study diseases in clinical trials that take years to pull together,” John said. “We don’t have that kind of time.”
For now, John said physicians are trying a few different drugs when treating severe cases of COVID-19. Those with mild or moderate cases are not receiving medication. But anyone who tests positive, no matter how mild or severe, is instructed to stay isolated for a period of time to avoid spreading the virus to others.
Researchers are also working to develop a vaccine, but it could take at least a year to be available for use. While the number of cases will hopefully decrease by then, Carlos said a resurgence of the virus is possible at some point.
“It’s important to develop a vaccine because if the virus becomes endemic, it may come back again after we've suppressed it this spring into the summer,” Carlos said. “It may come back again in the fall, winter or next spring. That's another active area of research and investigation and something I know all of medicine is really curious about.”
How do we stop it?
Health officials are urging people across the country to practice “social distancing” by staying home as much as possible and avoiding groups of 10 or more people in an effort to stop the rapid spread of COVID-19. Many employees are temporarily working from home and schools in Indiana are closed for weeks. But how temporary those arrangements are is still in question. While health officials hope the number of cases will begin to decrease soon, it could take weeks, or even months, to better contain the virus.
“It’s based on other countries’ data,” John said. “It takes a while for cases to decrease and you want them to come way down before you let up on what you’re doing or else you’ll have another spike.”
But not everyone is able to take part in social distancing, like those who work in grocery stores, restaurants continuing their drive-thru or carry-out service and health care providers.
“I think it's important for the community to remember that while everybody else is told to practice social distancing and to stay home with your family, we're asking our health care workforce to do the opposite,” Carlos said. “If there's less people that are out and about, there's less chance that those first responders, those people whose job it is to help others, will get sick.”
Spending less time out of the house also protects the elderly and those with underlying conditions who are more susceptible to COVID-19.
“This is something you do for other people,” Carlos said. “This is about people in nursing homes or people getting chemotherapy for cancer that are terrified of this virus.”
Physicians hope these measures will also help slow the spread of the virus and keep hospitals from becoming overwhelmed with too many patients at one time, because they won’t have the resources to help all the people they need to treat.
“I'm taking care of kids with infectious diseases that are not COVID-19, and those cases don’t stop,” John said. “We haven’t had a slowdown of people with other illnesses. People are still going to get sick.”
How to get through social distancing
While some may enjoy getting the opportunity to work from home or spending more time with loved ones, others may be experiencing loss of income, adjusting travel plans or just feeling stir crazy. The idea of social distancing can cause people to feel distant from others in more ways than just physical. That’s why Carlos would prefer we call it something else.
“I would prefer to say ‘physical distancing,’” Carlos said. “Humans are wired to live in relationships, and completely isolating yourself from others can create immense anxiety or even lead to depression. Utilize FaceTime and social media so you’re checking in with others and connecting. And just because you check in with someone on a Monday doesn't mean that you're good for the week. One day you might be doing fine and then you see a news story about a young person that died of coronavirus that was otherwise well and the next day you're ready to fall apart.”
“It’s one of the best times to show that we can be selfless and do good things for other people. There are many, many ways in which that can happen,” John said. “Groups are asking for people to help and it can be done in a way that is not in crowds and doesn’t put people at risk, but does help other people.”
“Don't emotionally distance, but do keep physical distance,” Carlos said. “We're counting on you in health care to do a good job so that we can do ours.”