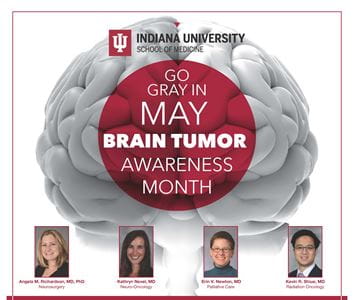
In recognition of Brain Tumor Awareness Month, four IU School of Medicine brain tumor specialists hosted “Go Gray in May,” a virtual question and answer session for brain tumor patients and their caregivers.
During the May 18 event, faculty physicians Angela M. Richardson, MD, PhD, Kathryn Nevel, MD, Erin V. Newton, MD, and Kevin R. Shiue, MD, addressed a wide range of concerns from brain tumor patients, including diagnosis, treatment and the palliative care support provided to patients by the IU team of specialists. Brain Tumor Awareness Month is dedicated to supporting, empowering and amplifying the voice of the brain tumor community.
“We wanted to bring more awareness and support to the Indiana community in terms of this disease,” explained Richardson, assistant professor of neurological surgery. “As a large academic center, we have access to clinical trials and specialists across the entire spectrum. From neuro-oncology and neurosurgery, radiation oncology, palliative care, rehabilitation medicine, otolaryngology, neuro-endocrinology, neuroradiology and neuropathology. Multi-disciplinary care is necessary for most brain tumor patients, and we’re fortunate to have an excellent team.”
An estimated 700,000 people in the U.S. are living with a primary brain tumor and approximately 88,900 will be newly diagnosed in 2022, according to the National Brain Tumor Society. Compared with other cancers, brain tumor is one of the rarest forms, with most tumors being diagnosed as benign. The lifetime risk of being diagnosed with a malignant brain tumor is less than 1%.
The general symptoms of brain tumor include headache, nausea, vomiting, blurred vision and seizures. Patients with a less aggressive or benign tumor might experience very mild forms of these symptoms for many months, said Nevel, assistant professor of clinical neurology. Experiencing these symptoms lead to patients to seek medical care and a tumor is discovered through brain imaging.
“With the commonness of CT scans and MRIs, however, patients sometimes are found to have brain tumors who don’t have any symptoms at all or who are getting a scan of their brain for another reason,” Nevel said. “For instance, if the individual was in a car accident and went to the emergency room and had a scan of their head to be sure there was no bleeding, a tumor may be discovered.”
Once a tumor is found, the multidisciplinary team of experts decide the best course of treatment and at different time points, the tumor may need different types of treatment.
“Brain tumors may not always be curable but we, as physicians, can always treat these patients, whether we’re able to remove the tumor, provide radiation therapy, give chemotherapy, provide symptom management or a combination of some or all of these,” Nevel said.
As a surgical neuro-oncologist, Richardson described the surgery options available to treat brain tumor, such as craniotomy, laser surgery and neuroendoscopy. “My conversations with patients typically start with discussing how the tumor was discovered, what their symptoms are and then evaluating what surgery can offer them,” she explained. “After surgery, patients return to Dr. Nevel or they often see Dr. Shiue if radiation is needed as an adjunct to treatment.”
Shiue, assistant professor of radiation oncology, provided an overview of brain tumor radiation treatment as high doses of daily radiation administered over several weeks. “Radiation is aimed at the area that we need to treat only, and while every treatment has side effects, I want patients to know that radiation treatment itself doesn’t hurt,” he said.
Newton then described her role as a palliative care specialist as “balancing hope with being practical.”
Her team includes a social worker, chaplain and nurse practitioner and they see patients who are approaching end-of-life but most of who are “are living quite well with their cancer.”
“If the brain tumor is going to be a person’s life-limiting condition, we want to make sure the time is as easy as possible,” said Newton, associate professor of clinical medicine.
Newton went on to advise that everyone, no matter their age or health status, should have a health care power of attorney and a legal will. The power of attorney allows patients’ appointed decision makers to make any decisions regarding their care when they may not have the capacity to do so. Patients can obtain palliative care services by requesting a referral from their neurosurgery care team, she explained.
Richardson also shared information about new brain tumor technology used by IU neurosurgeons, such as GammaTile therapy which involves placing radioactive tiles within the brain after a tumor is removed to target tumor cells immediately. Brain tumor patients in the Indianapolis region can also anticipate new brain tumor clinical trials opening at IU within the coming months.