Right Into the Fire
Matthew Harris Feb 01, 2016
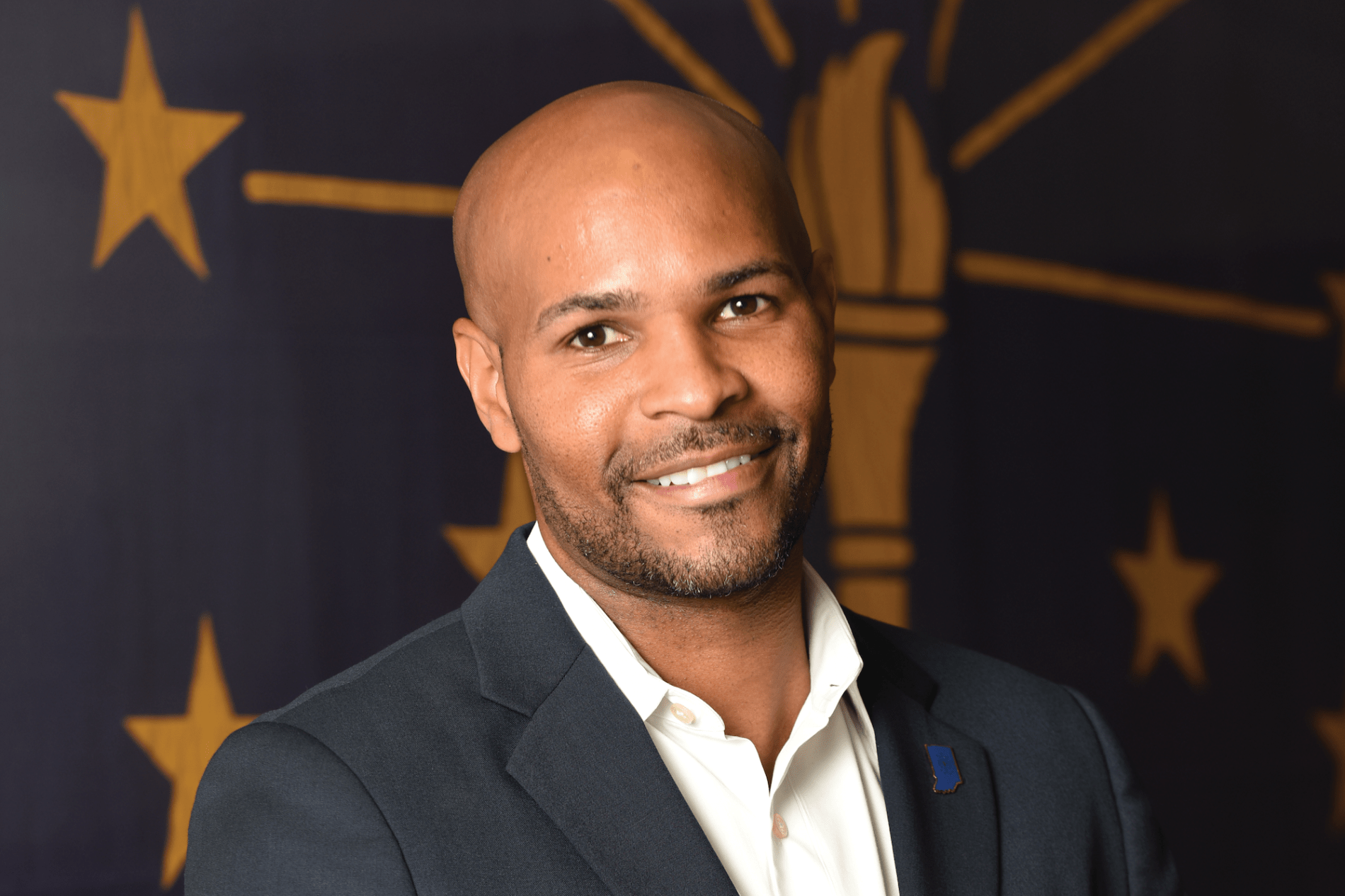
DR. JEROME ADAMS had little time to settle in after Gov. Mike Pence appointed him commissioner of the Indiana Department of Health in October 2014. Within six months, an outbreak of HIV, tied to needle-sharing among users of prescription pain killers, broke out in Scott County. Meanwhile, data from the Centers for Disease Control showed Indiana had the seventh-highest infant-mortality rate in the country, featuring a wide gap between white mothers and those who were black and Latino.
“I stepped right into the fire,” said Adams, a 2002 graduate of the Indiana University School of Medicine.
Ever since he was a medical student, Adams has been a proponent of applying policy and programs to impact the health of the population. During a fellowship abroad in Africa, he saw first-hand how futile it can be to treat patients long after they become ill. “If you waited, you were less successful than if you worked to keep people healthy in the first place.”
While he enjoys his role as an anesthesiologist, he realized that for every patient he helped, there were a dozen more he couldn’t treat. “It was absolutely necessary to do more than keep plugging holes in a dike,” he said.
What facets of medicine drew you in? What was the hook?
My parents were teachers, and I always wanted a career where I interacted with people. I majored in biochemistry and planned to complete my doctorate. But I worked in a lab with a gentleman who also did rounds. When you’re meeting with a patient, you’re educating them about their disease and improving their chances of overcoming the malady they’re facing at the moment.
You’re from Maryland and were recruited by a slew of top-flight medical schools out of college. What separated IU from those institutions?
IU did a great job putting together a competitive financial aid package. That’s important. Medical students accrue large debt. It doesn’t drive choice as the sole factor, but it’s there. IU also had deep ties to Eli Lilly and Company and other stakeholders. IU isn’t just an academic center. It values community and industry input.
Now as I travel, I see how deeply respected IU is for its clinical programs. At IU, you get so much diversity in settings and patients at the VA, Eskenazi Hospital, Riley Children’s Hospital and University Hospital.
You’re an anesthesiologist. Where do those roles intersect?
You convene people: Doctors, nurses, scrub techs, patients and their families. You bring them together to improve the health of the person having surgery. It’s the same in public health. You bring together diverse groups and convince them to be on the same team to improve health. There’s diversity, too. I may start the day with an 8-month-old patient and end with an 89-year-old patient. You’ve got to know a little bit of everything.
You split time between the operating room and keeping a state agency on track. Is there any crossover?
Working as a physician lends me credibility. I’m not ignorant to the reality of what’s going on in the real world and in our state. It’s hard for someone to question your advice on trauma care after you spent the night before on call taking care of someone in the operating room who has been shot multiple times.
As far as public health, I’m not hesitant anymore to bring up smoking or healthy eating with a patient. My job is to be an advocate and direct them to resources.
Gov. Mike Pence has his priorities. So does the state Legislature. And there are initiatives you feel are important. What’s an example of where those interests align?
Lowering the infant mortality rate is one. We’re at 7.1 percent, one of the nation’s worst rates. We told the governor, his wife and House Speaker Brian Bosma about the obstacles we face. Karen Pence helped unveil the Labor of Love campaign, and Speaker Bosma sponsored legislation to fund pilot projects aimed at lowering that number.
Starting a syringe-exchange program in Southern Indiana is another example. Indiana law doesn’t allow those. I explained to Gov. Pence they’re effective at halting the spread of infectious disease. We reached a consensus, and he signed an executive order for an exchange program to halt the HIV epidemic in that part of the state. I was proud he took that stance and that we could find space in the middle.
The state put forward $11 million to fund those infant-mortality programs. What objectives or projects is the department targeting?
We’ve looked at data from around the state to identify ZIP codes that are our largest contributors to infant mortality.
We’re targeting hospitals and community groups in those areas most affected. Those projects could address prenatal care, which is a major risk factor. There are also projects for safe sleep, which is one of the best ways to prevent infant mortality in our state.
The number of new HIV cases in Southern Indiana has leveled off. Systems are in place for testing, dispensing medication, treatment and exchanging needles. What lessons did you take away?
We all need to be more aware of what goes on around us. Physicians need to grasp there’s an opioid epidemic. It’s national. And it starts with over-prescribing. It’s not just doctors, but we all need to be aware we contributed to this breakout.
Eighty-percent of heroin users say their abuse started with prescription medications. We know the use of intravenous drugs is going up because hepatitis C rates are climbing. Indiana’s numbers have risen dramatically in the past decade.
We’ve also got to partner. We can’t do it alone. It includes working with church-based groups, community groups and law enforcement. As physicians, we usually don’t interact with those groups, but they were critical in Scott County.
The IU School of Medicine seems uniquely positioned to help. What role can it play moving forward?
We would not have been able to get this outbreak under control without the IU School of Medicine. It doesn’t just train physicians, and it doesn’t just play a role in the immediate area of its campuses.
In Scott County, the sheriff told me, “I want IU down here.” It’s a respected institution in the eyes of citizens. It establishes credibility and helps get over trust issues. They can see, “This is Indiana University. They’re going to do the right thing. I can trust what they’re telling me.”
Matthew Harris
Matthew Harris is a communications specialist in the Office of Gift Development. Before joining the School of Medicine in 2015, he was a reporter at newspapers in Pennsylvania, Arkansas, and Louisiana. He currently lives in Indianapolis with his wife and two basset hounds.