Orthopaedic surgeons hoping to use a common, minimally-invasive procedure to treat gunshot wounds to the hip must be aware that such surgeries come with a very high risk of complications, according to clinical research conducted by Indiana University School of Medicine faculty.
Physicians in the Department of Orthopaedic Surgery examined eight patients who suffered gunshot wounds to the hip.
To treat these injuries, the surgeons utilized arthroscopic debridement, which is a surgical method to remove damaged bone and fragments while keeping incisions small to lessen impact on the body. 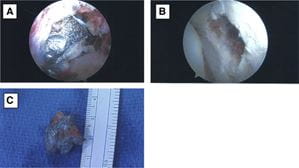
Full findings were published recently in ScienceDirect.
In five of the eight cases, surgeons reported poor visualization, for various reasons, making it difficult to view or access the bullet fragments. Two cases were converted to an open procedure, with doctors abandoning the minimally-invasive approach and opting for a large-incision surgery.
Based on the study’s results, while hip arthroscopy is a reasonable approach to treating this kind of trauma, surgeons who choose the approach must be aware of and consider the risks, said Brian Mullis, MD, a professor of orthopaedic surgery, who led the study.
Doctors also need to be prepared to convert to a more invasive surgery mid-procedure, which will likely lead to prolonged surgery times and risk further complications.
Mullis said the study’s findings made him more wary of choosing an arthroscopic debridement for hip gunshot wounds. Even surgeons who are well practiced in arthroscopic debridement are at high risk for complications when using the technique to treat gunshot wounds. Those with less experience using scopes may be better off using an open approach from the start.
Although the IU School of Medicine study focuses on only a handful of cases, it’s actually one of largest studies of its kind because the circumstance of a gunshot wound requiring arthroscopic debridement are fairly rare, said Mullis.
Jan Ertl, MD, an associate professor of orthopaedic surgery, participated in the study alongside Mullis. Two IU School of Medicine medical students also assisted in the research.
