By: Becca Koenigsberg, DO, PGY1
Sarah Bauer, MD, pediatric pulmonary fellow
Nadia Krupp, MD, associate professor of pediatrics
Key points:
- There have been 2,409 hospitalized cases of e-cigarette, or vaping, product-associated lung injury (EVALI) and 52 associated deaths reported to the Centers for Disease Control (CDC) as of December 10, 2019.
- Over half (54%) of cases have been in people less than 25 years old.
- Patients with EVALI may present similarly to the flu or pneumonia.
Currently, e-cigarettes and vaping are hot topics both in medicine and the media. E-cigarettes are electronic devices which heat a liquid to produce an aerosol which is then inhaled into the lungs of the user. The liquid can contain many different ingredients, including nicotine, tetrahydrocannabinol (THC), cannabinoid (CBD) oils, flavorings, and/or other unknown additives. Using an e-cigarette is commonly called “vaping.”
As of December 10, 2019, there have been 2,409 hospitalized cases of EVALI and 52 associated deaths reported to the CDC from all 50 states, Washington D.C, and 2 U.S. territories. Some of the highest rates of EVALI have been seen in the Midwest, including Wisconsin, Illinois, and Indiana. Use of THC-containing products, particularly when obtained from informal sources, have been linked to cases of EVALI and Vitamin E acetate has been identified as a “chemical of concern.” However, to-date there has not been one single etiology identified. In fact, there may be more than one cause and many other substances and products are under investigation.
As cases continue to increase nationwide, provider knowledge is imperative to identifying, treating, and counseling patients regarding e-cigarette and vaping products.
As medical providers, we hope our patients avoid or reject drugs and smoking, but the reality is that many adolescents and young adults avidly use e-cigarettes and vapes. According to the 2019 National Youth Tobacco Survey, over 5 million youths are currently using e-cigarettes. There continues to be a very concerning and dramatic increase in youth use of e-cigarettes. Among high school students, 1 out of every 3 to 4 students (27.5%) reports using an e-cigarette in the past 30 days and 10.5% of middle school students report the same. A growing population of adolescents are using e-cigarettes, becoming addicted to e-cigarettes, and, now, getting sick from e-cigarettes.
Providers must understand how EVALI presents, as the symptoms may mimic influenza and/or pneumonia. Importantly, EVALI is a diagnosis of exclusion, so a wide differential is crucial to identifying such patients. Patients are commonly presenting with respiratory, gastrointestinal, and constitutional symptoms such as cough, shortness of breath, nausea, vomiting, abdominal pain, fever, and fatigue. Many patients have presented to their primary care doctor prior to hospitalization.
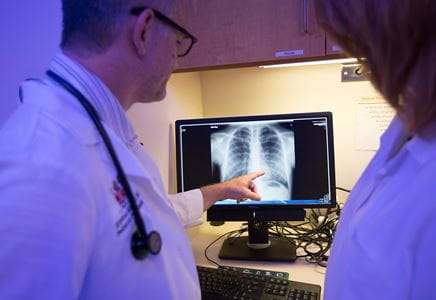
Our local experience in Indiana reflects the national experience with several of our hospitalized patients presenting as above. Often, they had previously been seen in the outpatient setting and diagnosed with an atypical pneumonia or viral illness. Their x-rays are often nonspecific and their clinical courses prior to presentation have been insidious. Some patients have quickly deteriorated once admitted and required positive pressure and/or invasive mechanical ventilation in the intensive care unit. We have seen several cases of pneumomediastinum and their chest CT scans have been consistent with other reported imaging findings nationwide of diffuse ground glass opacities often with sub-pleural sparing. To-date, the long-term consequences of EVALI are yet to be determined.
So how can we keep EVALI in mind when evaluating patients in the clinic? It is imperative to take a complete history regarding drug use. Once patients screen positive for vaping use, it is important to know the timeline (first use, last use), amount (number of cartridges, frequency), and type (THC vs nicotine vs both). If a patient has any respiratory symptoms, a history of vaping use within the past 90 days, and you suspect EVALI, a decision should be made as to whether outpatient versus inpatient care is indicated. According to the CDC, candidates for outpatient management should have: normal oxygen saturations, no respiratory distress, no comorbidities that may compromise pulmonary reserve, reliable access to care and a strong social support system, and be able to follow-up within 24-48 hours.
For clinicians following patients with a history of EVALI after hospitalization, it is important to counsel and encourage cessation and avoidance of e-cigarettes and vaping, screen for continued drug use, and treat any concomitant mental illness and/or withdrawal symptoms. Patients should also follow-up with a pulmonologist for pulmonary function testing and repeat imaging.
The CDC releases online updates weekly regarding any new information available. If you suspect an EVALI, call your local health department for information regarding reporting.