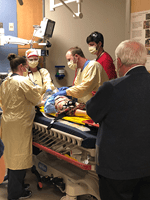
Photo: Drs. Sean Thompson, Will Martin, Emily Wagner, Kari Lemme
Coauthored by Kari Lemme, MD and Julie Welch, MD
“The goal is to make practice more difficult, physically/mentally than anything your players will face during a game.” -Coach Bob Knight
With the American pastime of viewing our beloved sports currently on furlough from the pandemic, we can still enjoy the many mantras born out of them to inspire us. Much like a basketball practice, rigorous development of new processes and procedures is alike to training for that critical moment of game-time. At Riley Children’s Hospital, the Division of Pediatric Emergency Medicine (PEM), has been fortunate to have many collaborative experiences to train for a new game, specifically, practicing pediatric emergency medicine in the era of COVID-19.
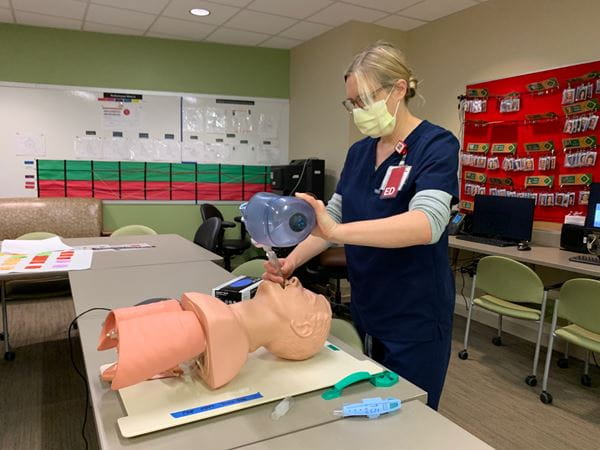
The Riley Emergency Department (ED) has been working in alliance with the Pediatric Intensive Care Unit (PICU) to develop their airway protocol. In a joint collaboration between the two specialties, there have been several in-situ airway simulations run in the Riley ED and the PICU. These airway simulations have been offered at variety of times during the day to accommodate different shift times. Through the process of these airway simulations, there has been ongoing learning for physicians, streamlining of process to ensure safety of all team members, and collective input from nursing, pharmacy and respiratory therapy on how to best implement guidelines with patient care. One of the biggest challenges was identifying how rapid sequence intubation (RSI), in the wake of COVID-19, differed from usual processes. Mock airway simulations have really helped work through these challenges. Dr. Anne Whitehead, PEM faculty, can attest to the impact of airway simulations: “I have had a couple of resuscitations at Riley since doing the airways sims and it was invaluable to have run through the process as a team beforehand. The medicine is the same, but every detail about how we practice has changed since COVID-19. It’s really important to be able to troubleshoot these processes before there’s a sick child in front of us.” Similarly, Dr. Elizabeth Weinstein, PEM Division Chief echoed, “Sims have been instrumental at helping us collectively problem solve challenges of resuscitating an ill child in the COVID-19 era. We have learned new skills and novel strategies and we have enhanced our team culture with critical input provided every step of the way by our RT’s, techs, RN’s pharmacists, unit secretaries and MD’s.”
The Riley ED has made other accommodations since the onset of the current pandemic. On March 23rd, Riley changed their work flow to help protect providers and patients, by splitting the ED into a PC (Potential COVID) and a Non-PC side of the department. The PC side is housed in the main ED, while the Non-PC side, with a separate entrance, is housed in the previous fast-track area. Patients currently undergo a sorting process outside the ED entrance at the former valet booth, and depending on their symptoms and exposure history, are sent to the appropriate side. This has allowed mindful appropriation of PPE and resources into the best spaces, as well as trying to keep patients and staff as safe as possible. Riley charge nurse, Tyler Hostetler, RN, feels "the process has been beneficial, especially as we have all become more medically informed. Information isn't changing as often as it was originally, we are better prepared about appropriate PPE, and there are more easily accessible resources to answer questions."
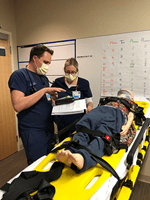
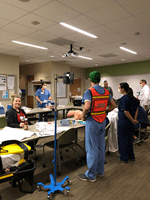
Riley underwent a multi-disciplinary trauma simulation case this week. The trauma simulation was a collaborative effort with the PEM, Trauma Surgery, and Infectious Disease. The goal of the simulation was to invite other disciplines into our space and identify the challenges that arise in managing a critical multi-system pediatric trauma patient with airway and invasive procedure needs within the confines of our negative airflow rooms. The exercise helped identify new airflow engineering needs that need to be explored for our current trauma bays. Dr. Brian Phillips, PEM faculty observed, “we were able to apply simulation in a way that both allowed our interdisciplinary team to drill and also help create an impetus to improve our process from a systems level. What we learned from this scenario will help us get the space and resources we need to continue toff the best pediatric care possible.” Dr. Tyler Arnold, Riley ED Assistant Medical Director, summarized, "With all of the changes in the COVID 19 era, sims have been necessary to quickly identify gaps in real-time, educate our staff, and ensure that we have the correct process and supplies for high risk procedures. These have fostered a team approach to problem solving, and moving forward, sims will hopefully be a part of our culture."
 |
 |
 |
 |
 |
The Riley ED has also been the benefactor of community generosity, coordinated by secretaries Rana Stultz and Deb Nickolson. Multiple businesses have provided incredibly thoughtful gestures such as food during various shifts, hand sanitizer, homemade headbands with button loops to tuck the face mask, and supportive encouragement in cards. A science teacher from Shelbyville donated protective eye wear. People have donated homemade masks for non-clinical areas, and made donations of PPE. Through social media, Dr. Holly Irwin, EM-Peds, PGY4, collected over 400 homemade protective hair-caps that have been donated to IEMS and Riley. These caps have been made by various groups throughout the state, such as Sew and Serve, as well as locally by pediatrics resident, Dr. Jessica Thoe.
 |
 |
Riley Children's Hospital leadership has maintained open communication with its faculty through a regular call-in meeting series on weeknight evenings to provide medical staff with COVID-19 updates. Dr. Brian Wagers, Physician Director of Pediatric and Maternal Quality and Safety, has been instrumental in leading these meetings, guiding medical staff through the presentation slides, moderating and answering questions, and bridging ED needs with Riley leadership. Riley leadership has worked with multiple hospitals throughout the state to decompress their pediatrics and transfer those patients to Riley, such as those from Methodist NICU and IU North Pediatrics, so that their hospitals can accommodate more adult COVID-19 patients. Nightly call-in chats are routinely tempered with praise to the medical staff for perseverance, excellence and innovation that has been shown throughout these challenging times.
Practice can only be effective if the team is unified. And a team is more than just its individual players. Riley ED Medical Director, Dr. Cory Showalter acknowledges the team approach at Riley. The team culture has always been a strength in the Riley ED, from inter-professional case reviews, debriefs, and ED councils on day-to-day interactions. There many people working tirelessly behind the scene to allow the Riley ED to adapt and function at top performance during the pandemic. Riley is currently seeing highest patient experience scores, with an 18-point improvement since March 2019, despite challenges of working behind impersonal PPE and palpable fear within the community. Among those behind the scenes include Security, who boosted staffing to secure the multiple ED entrances to ensure safety. Environmental Services has jumped to the challenge of enhanced deep cleaning of rooms and room capacity. Emergency Medicine administration has been working in the background to deliver ED support with data analysis, schedule changes, and complex payroll acrobatics. Tresanay Bentley, P-EMTC, has done an incredible amount of work in re-configuring our stocking and supply patterns. Clinical Nurse Manager Nettie Wilson, RN has been a critical piece of the glue holding the department together with daily operations updates for the department. PEM faculty, Dr. Heather Kelker has been serving as an integral part of the Wellness team for the Department of EM. Riley ED also celebrates the front-line caregivers who have defeated the virus and been able to safely return to work. Dr. Showalter recognizes the efforts of all and is grateful for “every single doctor, nurse, RT, tech, medic, secretary, EVS, pharmacist, who makes the choice to come to work and sacrifice comfort and risk exposure to take care of children across this state...we are a TEAM and that’s the only way we have been able to thrive in this environment.”
We have all found ourselves learning in real time, digesting new material as quickly as it comes out. Terms such as I-gel, AGP’s, appropriate PPE, and viral filters have found their way into routine ED vocabulary where they didn’t have much merit six weeks ago. These new “plays” will ensure our offense is ready when the time comes. Each passing week brings more confidence and comfort in new process utilization. These key steps of practicing will make “game time” that much smoother. Although outfitted in scrubs instead of candy stripes, and ID badges in place of numbered jerseys (I’d pick #23), the team at Riley PEM is unified and preparing daily. Coach Knight would be proud.
